CASE REPORT |
https://doi.org/10.5005/jp-journals-10045-00202 |
Spontaneous Splenic Rupture during Pregnancy: A Rare Entity
1-3Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India
4Department of General Surgery, Government Medical College and Hospital, Chandigarh, India
Corresponding Author: Sunita Dubey, Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India, Phone: +91 9646323268, e-mail: sunitas504@gmail.com
ABSTRACT
Background: Spontaneous splenic rupture during pregnancy is usually misdiagnosed as abruptio placentae and uterine rupture.
Case description: A 35-year-old G2P1L1 with a previous cesarean section at 38 weeks of gestation was referred to our emergency obstetrics department with a diagnosis of uterine rupture. She had sudden onset of epigastric pain following lifting of a heavy container without any direct trauma on her abdomen. Severe pallor with tachycardia was there on examination. She did not complain of labor pains. Uterine contour could not be made out due to guarding; however, it was found intact on bedside transabdominal ultrasonography, a large amount of free fluid and fetal demise without any evidence of retroplacental clots was also confirmed. She was taken up for emergency laparotomy. Massive hemoperitoneum due to splenic rupture was evident during laparotomy, the site of rupture was covered with hematoma with an absence of active bleeding thus left undisturbed. She received multiple blood transfusions with successful recovery.
Conclusion: Sudden epigastric pain, pallor, and hypotension following abdominal strain may be a sign of splenic rupture. Resuscitation of patients with immediate laparotomy should be done in these patients to avoid fetal and maternal morbidity and mortality.
Key message: Sudden epigastric pain with pallor and hypotension following abdominal strain may be a sign of splenic rupture. Hence, it should be one of the differential diagnoses in addition to abruptio placentae and scar rupture in suspected hemorrhagic shock. Resuscitation of patients with immediate laparotomy should be done in these patients to avoid fetal and maternal morbidity and mortality.
How to cite this article: Dubey S, Rani P, Gupta V, et al. Spontaneous Splenic Rupture during Pregnancy: A Rare Entity. J Med Sci 2021;7(2):32-34.
Source of support: Nil
Conflict of interest: None
Keywords: Hemorrhagic shock, Organ rupture, Rupture uterus, Splenic rupture
BACKGROUND
Spontaneous splenic rupture is a rare and life-threatening entity, especially during pregnancy. As it occurs without obvious trauma, delayed diagnosis and treatment can lead to fetal and maternal morbidity and mortality. It has been reported even following trivial abdominal straining where the diagnosis was made during laparotomy only. This case is brought for discussion due to scanty literature and to increase the awareness of treating physicians when to suspect life-threatening splenic hemorrhage to avoid grave fetal and maternal complications.
CASE DESCRIPTION
A 35-year-old G2P1L1 at 38 weeks gestation was referred from a civil hospital with a diagnosis of uterine rupture. She gave a history of pain in the epigastric region after lifting a heavy bucket followed by decreased fetal movements from 8 hours. She did not give any history of labor pains and abdominal trauma. There was no history of fever and vomiting. There was no history of increased blood pressure. Her past, medical, and family history were not significant. Obstetric history- she had one lower segment cesarean section 6 years back because of fetal distress and delivered an average size female baby. The postoperative period was uncomplicated.
On examination, she was conscious but had mild restlessness too. Clinically, she was pale with hemoglobin of about 2 g/dL. Her pulse rate was 130/minute with low volume and her blood pressure was 124/80 mm Hg. The respiratory rate was 30/minute. However, the chest was clear on auscultation. Her abdomen was tense and tender with guarding and rigidity. The fetal heart was not audible with a stethoscope. Uterine contour was indistinguishable due to guarding. On vaginal examination, the cervix was 2 cm dilated, uneffaced with intact amniotic membranes, and presenting part was high up. Clear urine was drained on catheterization of the bladder.
Bedside transabdominal ultrasonography revealed a single intrauterine fetus with absent cardiac activity, and there was no evidence of retroplacental hematoma. Uterine contour was well maintained. Free fluid was seen in the paracolic gutter and bilateral subphrenic region. Preoperative blood investigations revealed hemoglobin of 5.0 g/dL, prothrombin index (PT) was 74% and platelets were 2.21 lac/µL with raised total leukocyte (TLC) count of 24000 cells/mm3. Renal and liver function tests were within normal limits. Arterial blood gas analysis revealed metabolic acidosis.
Along with resuscitation, she was taken up for emergency laparotomy because of suspected intra-abdominal hemorrhage; the abdomen was opened by a midline vertical incision. Intraoperatively hemoperitoneum was confirmed. A fresh stillborn baby of 2 kg was delivered by lower segment cesarean section. There was no uterine rupture, bilateral ovary, and fallopian tubes were healthy. To know the site of hemorrhage, a midline incision was extended above the umbilicus. The upper abdomen was explored by a general surgeon. There was a large collection of blood clots in the left upper abdomen near the perisplenic area; therefore, the left side was explored first, on the removal of clots splenic rupture of 2 × 2 cm size was seen over the superior surface with a small clot over it which was left undisturbed (Fig. 1). Another laceration of 5 × 1 cm was seen over the inferior surface of the spleen. Splenic hilum was normal. The liver and other organs were also normal. A total of 2-l hemoperitoneum and 740-g clots were removed. The intraabdominal drain was kept to look for ongoing bleeding. Total four units of packed red blood cells and four units of fresh frozen plasma were transfused. She was given antibiotics and milk suppressants. After surgery, her vitals were monitored in a high dependency unit (HDU). The postoperative period was uneventful. She was discharged on the 7th day of surgery with the advice to take hematinic. Her hemoglobin (Hb) level was 7.9 g/dL, platelets were 1.80 lac/μL and TLC was 19000 cells/mm3 at the time of discharge.
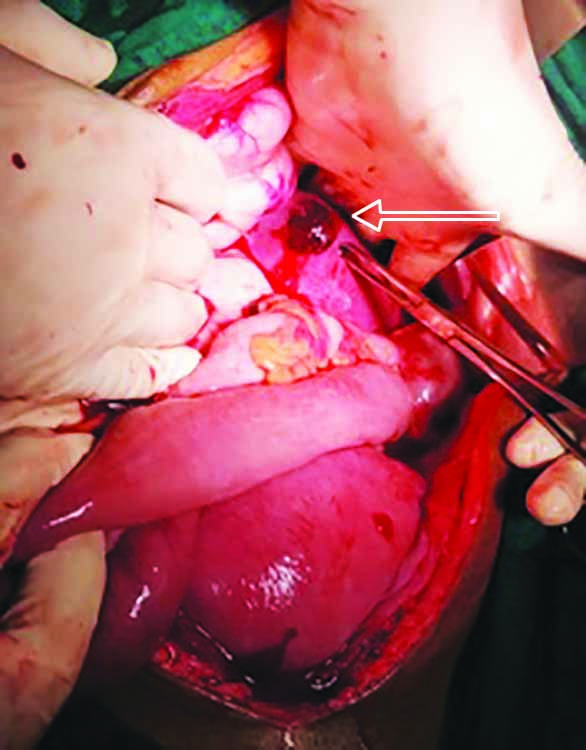
Fig. 1: Intraoperative photograph showing the splenic rupture of about 2 × 2 cm size over the superior surface with small clot over it
DISCUSSION
Spontaneous atraumatic rupture of the spleen is a rare event, whereas trauma is the major reported cause of splenic rupture in adults. Various etiologies of nontraumatic splenic rupture have been reported; however, abnormal coagulation, infections, and malignancies contribute to the majority of splenic rupture.1 Out of all nontraumatic causes, only 6.4% of cases were described in the normal spleen.2 While, its incidence during pregnancy has never been reported due to extremely rare entity. Splenic rupture during early pregnancy has been reported in splenic ectopic pregnancy and in advanced pregnancy with preeclampsia as a result of endothelial damage and thrombosis.3,4 However, spontaneous splenic hematoma without any underlying cause is rarely reported during pregnancy leading to the wrong diagnosis of abruptio placentae and uterine rupture.5,6
Rupture of normal-sized spleen without any underlying cause, trauma, and adhesions are the criterion of spontaneous splenic rupture. During pregnancy, splenic rupture has been correlated with decreased peritoneal space with constantly increasing splenic and uterine size with advanced gestation. The spleen becomes more fragile due to vascular congestion as a result of raised plasma and erythrocytes levels following a significant increase in maternal blood volume, especially in twins and the third trimester. The risk of splenic rupture is further increased due to compression by abdominal musculature while an increase in intraabdominal pressure following minimal strain like coughing, sneezing.7 While lifting a heavy bucket was the preceding event in the present case. Although, left shoulder tip pain was reported in 50% of patients instead pain was initially localized to the epigastric region in the present case.8,9 Signs of pallor and tachycardia are usually followed by hemorrhagic shock whereas hypotension was not present in this case as a result of an early visit to the primary health center, and timely referral from there with ongoing intravenous fluid replacement and spontaneous cessation of bleeding from rupture site also helped in rapid resuscitation. However, due to sudden massive hemoperitoneum intrauterine fetal demise could not be prevented in the present case.
Along with resuscitation of the patient, bedside ultrasonography can help in defining uterine contour, free fluid, and placental hematoma as we did in the present case. However, the use of ultrasound or any imaging modality should not delay definitive management. As delayed management leads to more complications like hemorrhagic shock, intrauterine fetal demise, disseminated intravascular coagulation (DIC), and the need for intensive care.
Management of splenic rupture depends on the clinical condition of the patient, underlying pathology, and grade of injury.10 Conservative management should be followed by intensive monitoring in HDU with the facility of frequent clinical and laboratory evaluation, round the clock availability of intervention radiologist, surgeon, and blood products. Otherwise, urgent exploratory laparotomy should be aimed to conserve the spleen by repair of capsule, splenorrhaphy, and partial splenectomy, ligation of splenic vessels should be tried before splenectomy in patients showing good response to blood transfusion as splenectomy may increase the risk of frequent infections and overall morbidity and mortality. Hence, patients should be compliant with vaccine prophylaxis.11 As vessels are running over the inferior costal margin; exploration should be avoided at this place to avoid damage to intercostal vessels. The use of transcatheter arterial embolization (TAE) should be considered in a stable patient responding to volume replacement.
CONCLUSION
Sudden epigastric pain with unstable vitals following trivial abdominal strain or trauma may be a sign of splenic rupture. Obstetricians must be aware of this entity- resuscitation, early referral, and immediate emergency cesarean section can avoid intrauterine fetal demise and maternal morbidity.
ORCID
Pooja Rani https://orcid.org/0000-0002-8274-1640
REFERENCES
1. Tonolini M, Ierardi AM, Carrafiello G. Atraumatic splenic rupture, an underrated cause of acute abdomen. Insights Imaging 2016;7(04):641-646. DOI: 10.1007/s13244-016-0500-y
2. Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96(10):1114-1121. DOI: 10.1002/bjs.6737
3. Greenbaum A, Miskimins R, Coffman B, et al. Management of splenic ectopic pregnancy presenting with massive haemoperitoneum. BMJ Case Rep 2016;2016:bcr2016218291. DOI: 10.1136/bcr-2016-218291
4. Hamedi B, Shomali Z. Postpartum spontaneous rupture of spleen in a woman with severe preeclampsia: case report and review of the literature. Bull Emerg Trauma 2013;1(01):46-48.
5. De Graaff J, Pijpers PM. Spontaneous rupture of the spleen in third trimester of pregnancy. Report of a case and review of the literature. Eur J Obstet Gynecol 1987;25(03):243-247. DOI: 10.1016/0028-2243(87)90105-5
6. Bhartiya V, Sharma R. Splenic hematoma mimicking rupture uterus: a diagnostic dilemma. Int J App Basic Med Res 2018;8(02):132-134. DOI: 10.4103/ijabmr.IJABMR_458_16
7. Lemon M, Dorsch M, Street K, et al. Splenic rupture after vomiting. J R Soc Med 2001;94(10):527-528. DOI: 10.1177/014107680109401012
8. Foreman BH, Mackler L, Malloy ED. Can we prevent splenic rupture for patients with infectious mononucleosis? J Fam Pract 2005;54(06):547-548.
9. Looseley A, Hotouras A, Nunes QM, et al. Atraumatic splenic rupture secondary to infectious mononucleosis: a case report and literature review. Grand Rounds e-med 2008;9:8-9. DOI: 10.1102/1470-5206.2009.0002
10. Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017;12:40. DOI: 10.1186/s13017-017-0151-4
11. Davies JM, Lewis MPN, Wimperis J, et al. British Committee for Standards in Haematology. Review of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen: prepared on behalf of the British Committee for Standards in Haematology by a Working Party of the Haemato-Oncology Task Force. Br J Haematol 2011;155(03):308-317. DOI: 10.1111/j.1365-2141.2011.08843.x. PMID:
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.